Scientific Calendar October 2025
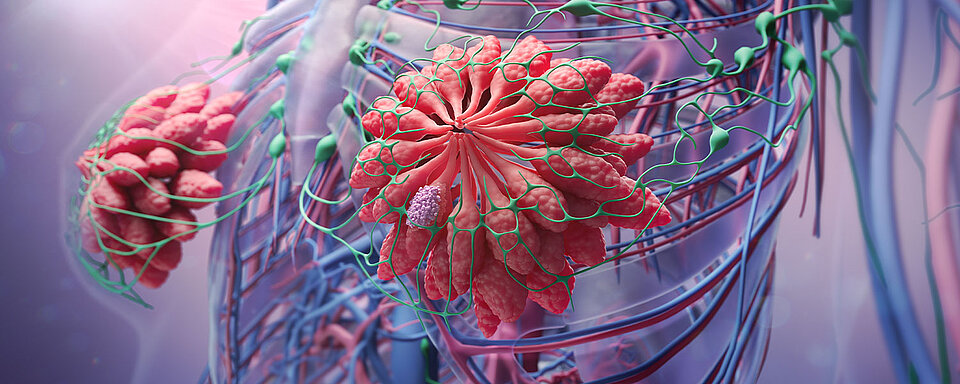
Hereditary breast cancer – how genetic and molecular testing can support prevention and early cancer diagnosis
Do you know what the risk of developing breast cancer is when one is a carrier of BRCA mutations?
50-60% depending on the BRCA variant
50-80% depending on the BRCA variant
40-60% depending on the BRCA variant
40-80% depending on the BRCA variant
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Patient Story - part 1
After her sister’s recent breast cancer diagnosis, a young woman decided to take her health into her own hands. Being a mother, she understood the importance of testing for hereditary breast cancer and with encouragement from a genetic counsellor, she underwent germline blood testing. Unfortunately, the results came back positive for BRCA1 mutation.
Due to the increased risk of developing cancer associated with it, her gynaecologist recommended her taking more vigilant action. In addition to mammography, the doctor proposed to increase the frequency of her check-up visits and include magnetic resonance imaging (MRI).
Just two years later, a small mass was detected in her right breast during one check-up. The biopsy and the molecular subtyping by MammaTyper® confirmed invasive triple-negative breast cancer.
This is an example of how genetic and molecular testing can support early cancer detection. For some patients, the battle against breast cancer starts long before the initial diagnosis.
This was the story so far, as published in the printed version of the Sysmex Scientific Calendar. If you are interested in learning more about the patient’s story, please continue reading.
Patient Story - part 2
After the young woman was diagnosed with triple-negative breast cancer, she was recommended to undergo neoadjuvant systemic treatment. This recommendation was made due to the rather aggressive type of cancer, despite her tumour being smaller than 2 cm in size.
Wishing to become a mother once more after completing cancer treatment, the patient decided to have her oocytes collected and frozen before starting treatment.
Following completion of systemic treatment, imaging analysis showed shrinkage of the tumour, which could then be completely removed through surgery. During the same procedure, the sentinel lymph nodes were excised and analysed using the OSNA method. Fortunately, the nodes showed no metastasis.
After the young woman was cured of breast cancer, she decided to pursue her motherhood plans and underwent in vitro fertilisation. This successfully led to the birth of her second child, a daughter.
The patient’s story concludes 25 years later on a positive note: both her children have undergone blood tests for hereditary cancer, and the results for both were negative – neither carries the pathogenic BRCA mutations.
Scientific background
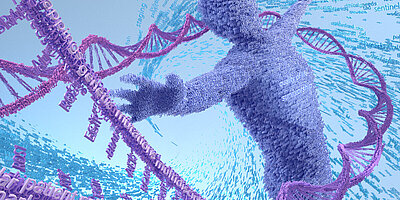
BRCA1 and BRCA2 proteins in DNA damage response and cancer risk (1,2)
BRCA1 and BRCA2 proteins are essential in the cellular DNA damage response (DDR), facilitating the conservative repair of DNA double-strand breaks through the homologous recombination repair pathway.
Loss-of-function mutations in the BRCA1 and BRCA2 genes, caused by somatic mutations or epigenetic silencing, result in cells becoming reliant on alternative, error-prone, lower-fidelity DNA repair mechanisms, leading to potential genomic instability and tumourigenesis.
Mutations in BRCA1 and BRCA2 are inherited in a dominant fashion. Although typically only one mutated allele is passed down, this is sufficient to significantly elevate cancer risk due to the resulting impairment in DNA repair capacity.
Hereditary breast and ovarian cancer syndrome (HBOC) (1)
Hereditary breast and ovarian cancer syndrome (HBOC), caused by a germline pathogenic variant in BRCA1 or BRCA2, is characterised by an increased risk for several malignancies. These include breast, fallopian tube, primary peritoneal and ovarian cancers in females, as well as pancreatic, colorectal cancer, melanoma, prostate and male breast cancer.
Table 1: The estimated lifetime risk for individuals with a pathogenic BRCA1 or BRCA2 variant
| Cancer type | General population risk | Mutation risk BRCA1 & BRCA2 |
| Breast | 12% | 40%–80% |
| Ovarian | 1%–2% | 11%–40% |
| Male breast | 0.1% | 1%–10% |
| Prostate | 15%–18% | up to 39% |
| Pancreatic | 0.5% | 1%–7% |
References
[1] BRCA1 and BRCA2 in Ovarian Cancer: (2025): ESMO Biomarker Factsheet | OncologyPRO
[2] Arun B et al. (2024): British Journal of Cancer; 131:1400–1414.