Scientific Calendar January 2020
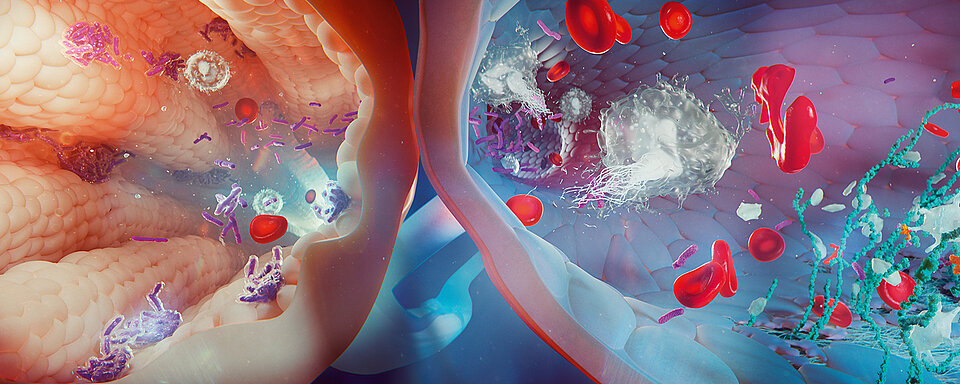
Cancer and thrombosis
Which type of cancer is showing the highest risk of VTE during systemic treatment?
Colon cancer
Pancreatic cancer
Breast cancer
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific background
Cancer-associated venous thromboembolism (VTE) is the second largest common cause of death in cancer patients after the cancer itself. Cancer patients may have a four- to seven-fold increased risk of VTE compared with the general population. The risk varies considerably from patient to patient and is based on factors such as the malignancy itself, treatment and patient-associated features as shown in Table 1.1, 2
Table 1 Risk factors for cancer-associated VTE
GROUP | RISK FACTOR |
| Cancer-associated risk factors | |
| Tumour site and size | |
| Tumour stage and grade | |
| Time interval after diagnosis (up to six months) | |
| Treatment-associated risk factors | |
| Chemo- and radiotherapy | |
| Hormonal therapy | |
| Indwelling intravenous catheters | |
| Surgery | |
| Antiangiogenic agents | |
| Patient-associated risk factors | |
| Age | |
| Ethnicity | |
| Gender | |
| Life style-related risk factors, i.e. smoking, obesity or immobility | |
| Hormonal status | |
| History of thrombosis |
Certain types of cancer show a higher probability of developing VTE than others. However, breast cancer is the entity with the greatest risk of VTE, which usually arises during systemic treatment.3
Changes in physiologic parameters such as elevated platelet and WBC counts, or reduced haemoglobin levels were shown to be indicative of chemotherapy-associated VTE.2
Another parameter broadly used is D-dimer, but the incidence of VTE related to elevated D-dimer levels varies among the different cancer types, with the highest found in colorectal cancer patients compared to others (one-year incidence of DVT 20% (95% CI, 12–31%) vs 5% (95% CI, 2–12%), respectively).4 In breast cancer patients, levels of D-dimer are higher in patients with axillary lymph node involvement compared to patients without.5 Another biomarker that might reflect the risk of VTE in breast cancer is the thrombin-antithrombin (TAT) complex in plasma, which is elevated like D-dimer.6
Tissue factor (TF), the physiologic activator of haemostasis and identified as a promoter of cancer stem cell activity, is also elevated in cancer patients and released into the circulation in the form of microparticles. Assays to assess the TF include immunohistochemical grading of TF expression on tumour cells, measurement of TF antigen using ELISA [e.g. ZYMUTEST™ Total Tissue Factor (RUO); Hyphen Biomed, A Sysmex Group Company; Neuville-sur-Oise, France], TF microparticle procoagulant activity [e.g. ZYMUPHEN™ MP-TF (RUO); Hyphen Biomed, A Sysmex Group Company; Neuville-sur-Oise, France] or flow cytometry. Studies indicate an association between elevated TF and VTE, but this is limited to certain tumour sites and stages (pancreatic and ovarian cancer) only and cannot be used for overall prediction.2
Prothrombin fragment F 1+2, urokinase-type plasminogen activator (uPA) and plasminogen activator inhibitor-1 (PAI-1) are also associated with elevated VTE risk, but their predictive value is controversial among different studies.7, 8, 9 Table 2 summarises the incidence of abnormal coagulation biomarkers in cancer patients.
Table 2 Incidence of abnormal coagulation biomarkers in cancer patients of diverse entities
BIOMARKER | INCIDENCE (%) | REFERENCE RANGE |
| D-dimer | 50 – 90 | ≤ 0.5 mg/L FEU |
| Fibrinogen | 40 – 80 | 1.7 – 4.2 g/L |
| TAT complex | 40 – 70 | < 4 ng/mL |
| FDP | 60 – 80 | < 10 µg/mL |
| Prothrombin fragment 1+2 | 35 – 55 | 0.069 – 0.229 nmol/L |
| Thrombocytosis | 5 – 80 | 150 – 350 x 109/L |
Biomarkers support the prediction of the risk of developing VTE; however, careful patient assessment and management is essential for preventing it. Therefore, several predictive models have been established which consider levels of certain biomarkers as well as the type of cancer and other patient characteristics to support clinicians in VTE prevention. The best-known model after Khorana et al. is shown in Table 3.2
Table 3 Predictive model for chemotherapy-associated VTE
PATIENT CHARACTERISTICS | SCORE |
| Cancer entity | |
| Very high risk (stomach, pancreas) | 2 |
| High risk (lung, lymphoma, gynaecologic, bladder, testicular) | 1 |
| Pre-chemotherapy platelet count ≥ 350 x 109/L | 1 |
| Haemoglobin concentration < 100 g/L or use of erythropoiesis-stimulating agents | 1 |
| Pre-chemotherapy leucocyte count > 11 x 109/L | 1 |
| Body mass index ≥ 35 kg/m2 | 1 |
High-risk score: ≥ 3; intermediate risk score: 1–2; low-risk score: 0
Identification of novel VTE-associated biomarkers in individual malignancies is required to drive the development of cancer type-specific scoring systems with an improved predictive value.
References
[1] Blom JW, Doggen CJ, Osanto S, Rosendaal FR. (2005): Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA 293(6):715–722.
[2] Alok A. Khorana. (2012): Cancer and Coagulation. Am J Hematol 87:S82–S87.
[3] Cohen AT, Katholing A, Rietbrock S, Bamber L, Martinez C. (2017): Epidemiology of first and recurrent venous thromboembolism in patients with active cancer. A population‐based cohort study. Thromb Haemost 117(1):57–65.
[4] Stender MT, Frokjaer JB, Larsen TB et al. (2009): Preoperative plasma D-dimer is a predictor of postoperative deep venous thrombosis in colorectal cancer patients: A clinical, prospective cohort study with one-year follow-up. Dis Colon Rectum 52:446–451.
[5] Blackwell K, Haroon Z, Broadwater G, Berry D, Harris L, Iglehart JD et al. (2000): Plasma d-dimer levels in operable breast cancer patients correlate with clinical stage and axillary lymph node status. J Clin Oncol 18(3):600–608 (PubMed PMID: 10653875).
[6] Topcu TO, Kavgaci H, Canyilmaz E, Orem A, Yaman H, Us D et al. (2015): The effect of adjuvant chemotherapy on plasma TAT and F 1 + 2 levels in patients with breast cancer. Biomed Pharmacother 73:19–23 (PubMed PMID: 26211577).
[7] Lampelj et al. (2015): Urokinase plasminogen activator (uPA) and plasminogen activator inhibitor type-1 (PAI-1) in breast cancer – correlation with traditional prognostic factors. Radiol Oncol 49(4): 357-364.
[8] Völker et al. (2018): Levels of uPA and PAI-1 in breast cancer and its correlation to Ki67-index and results of a 21-multigene-array. Diagnostic Pathology 13:67.
[9] Ferroni et al. (2014): Plasma Plasminogen Activator Inhibitor-1 (PAI-1) Levels in Breast Cancer – Relationship with Clinical Outcome. ANTICANCER RESEARCH 34:1153–1162.
[10] Mandoj et al. (2018): Observational study of coagulation activation in early breast cancer: development of a prognostic model based on data from the real world setting. J Transl Med 16:129.