Bladder cancer diagnostics and surveillance
Urothelial carcinoma, also known as transitional cell carcinoma (TCC), is the most common type of bladder cancer. It starts in the urothelial cells that line the inside of the bladder and its initial diagnosis often coincides with the presence of related symptoms at later stages of the tumour growth. This negatively affects the chance of healing and requires invasive procedures, such as partial or complete resection of the bladder. Since urothelial carcinoma show a high rate of remission, close monitoring of treated patients is mandatory by up to four invasive cystoscopies, yearly.
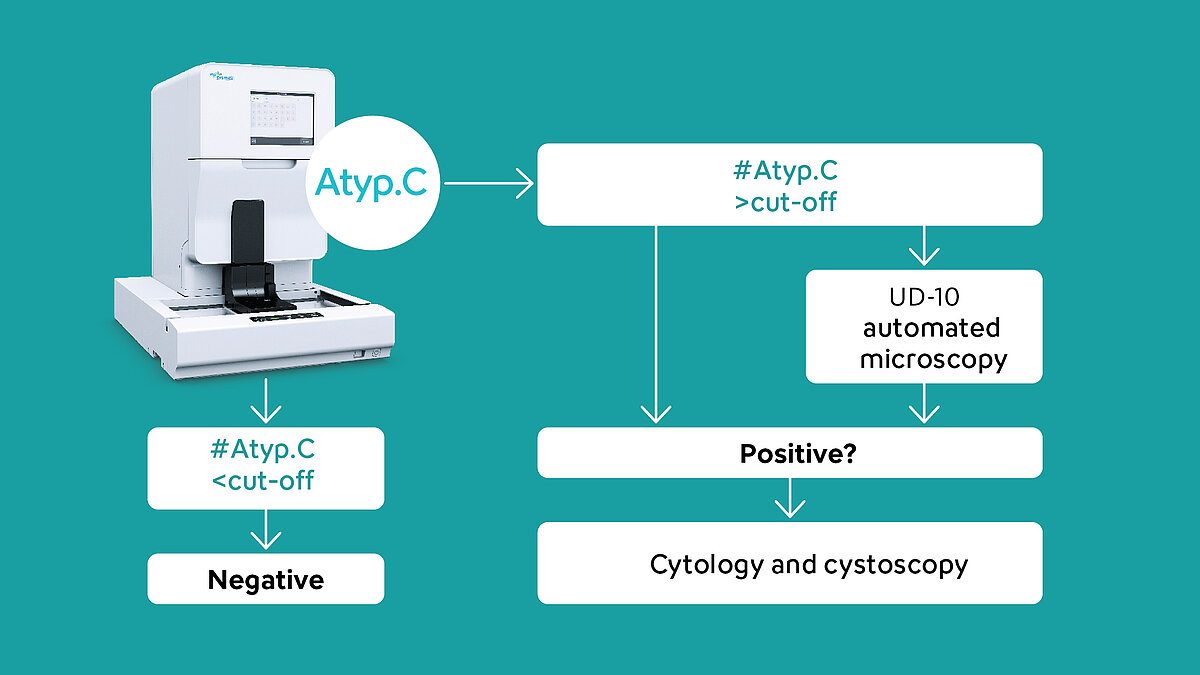
The detection of urinary atypical cells using the research parameter Atyp.C bears the potential to detect malignant cells at early stages and to reduce unnecessary invasive cystoscopies.
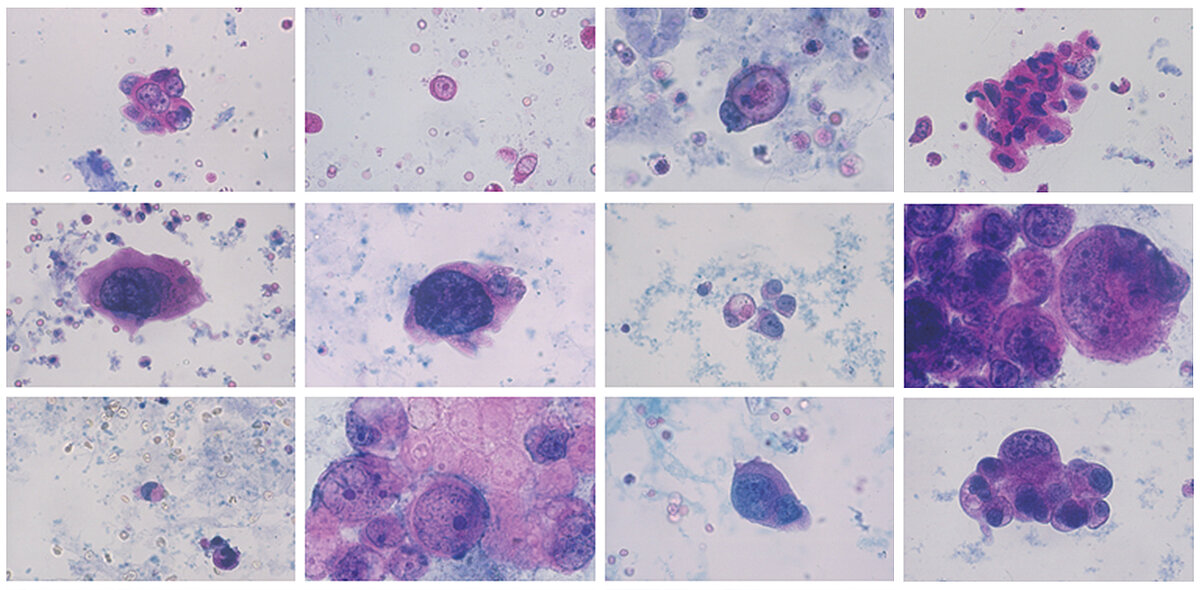
Urinary atypical cells
Atypical cells with changes or cells that are suspected of malignancy are released from urothelial tissues through exfoliation and show the one or another morphological feature, which can include:
- Enlarged nucleus > 25 µm
- Increased N:C (nucleocytoplasmic) ratio > 80 %
- Irregular shape
- Hyperchromasia
- Irregular chromatin patterns
- Nucleolic hypertrophy > 5 µm
- Increased number of nucleoli
- Irregular nuclear shape
- Appearance of cellular masses
How to detect atypical cells in urine?
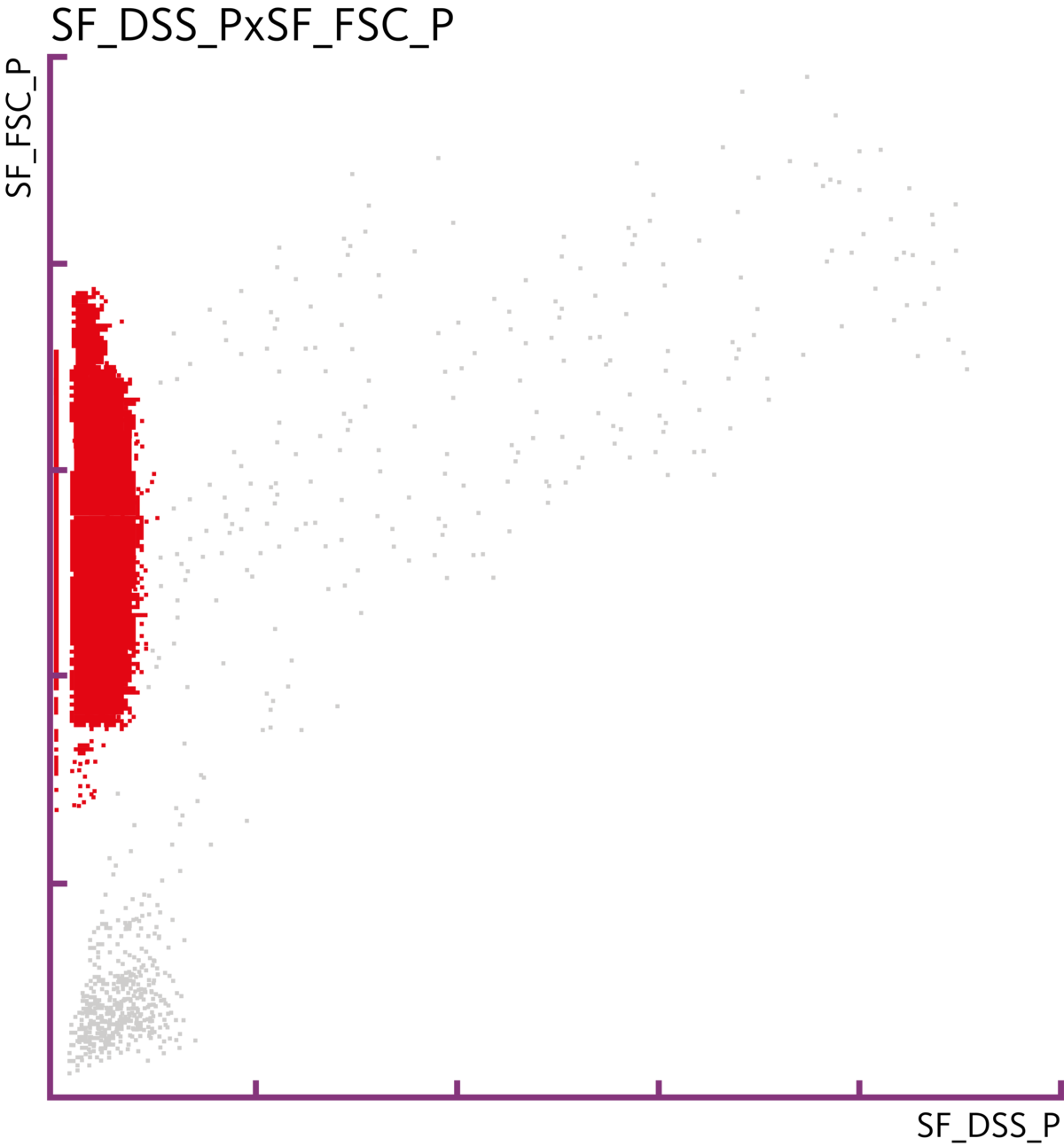
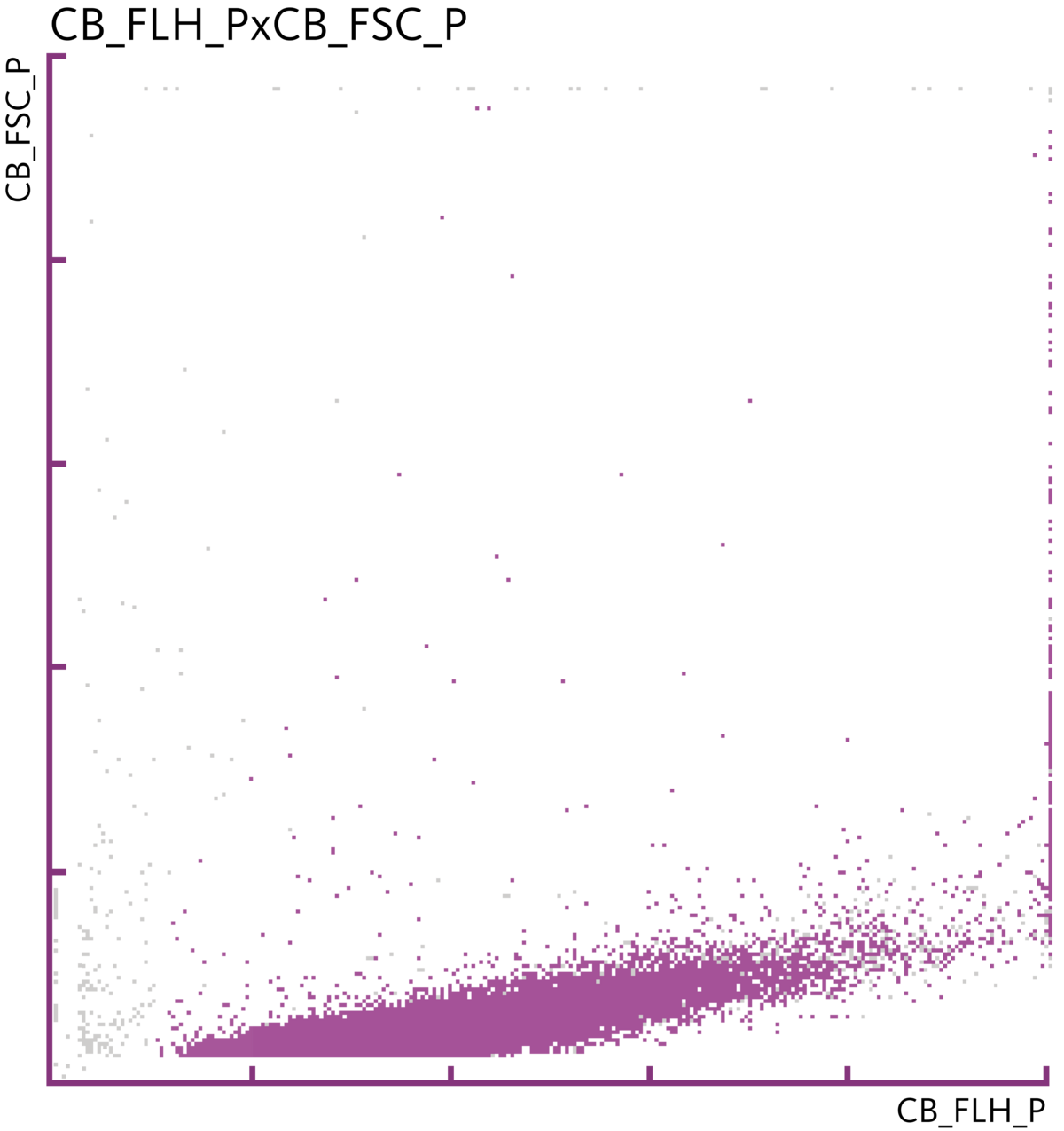
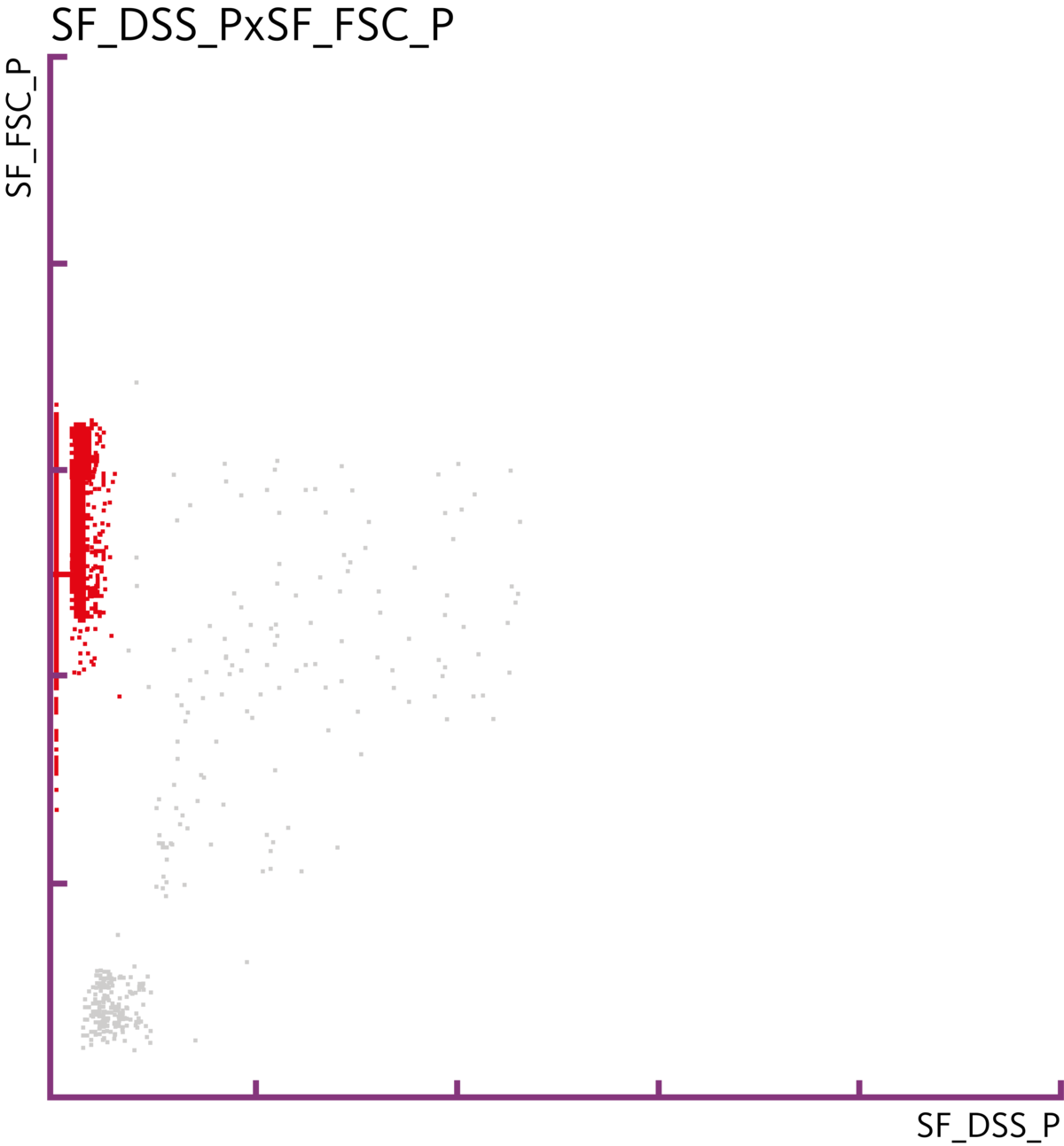
Urinary flow cytometry uses specific fluorochromes for the staining of surface structures and nucleic acid content of cellular urinary particles. Stained cells are injected into a flow cell after hydrodynamic focusing to allow the detection of individual cells and to ensure high accuracy.
Upon laser scanning collection on number of cells, internal cellular structures, cellular volume and nuclear characteristics, the result is particle-dependent emission signals, which are then assigned into a three-dimensional scattergram. Through dedicated algorithms, detected cells are identified and quantified.
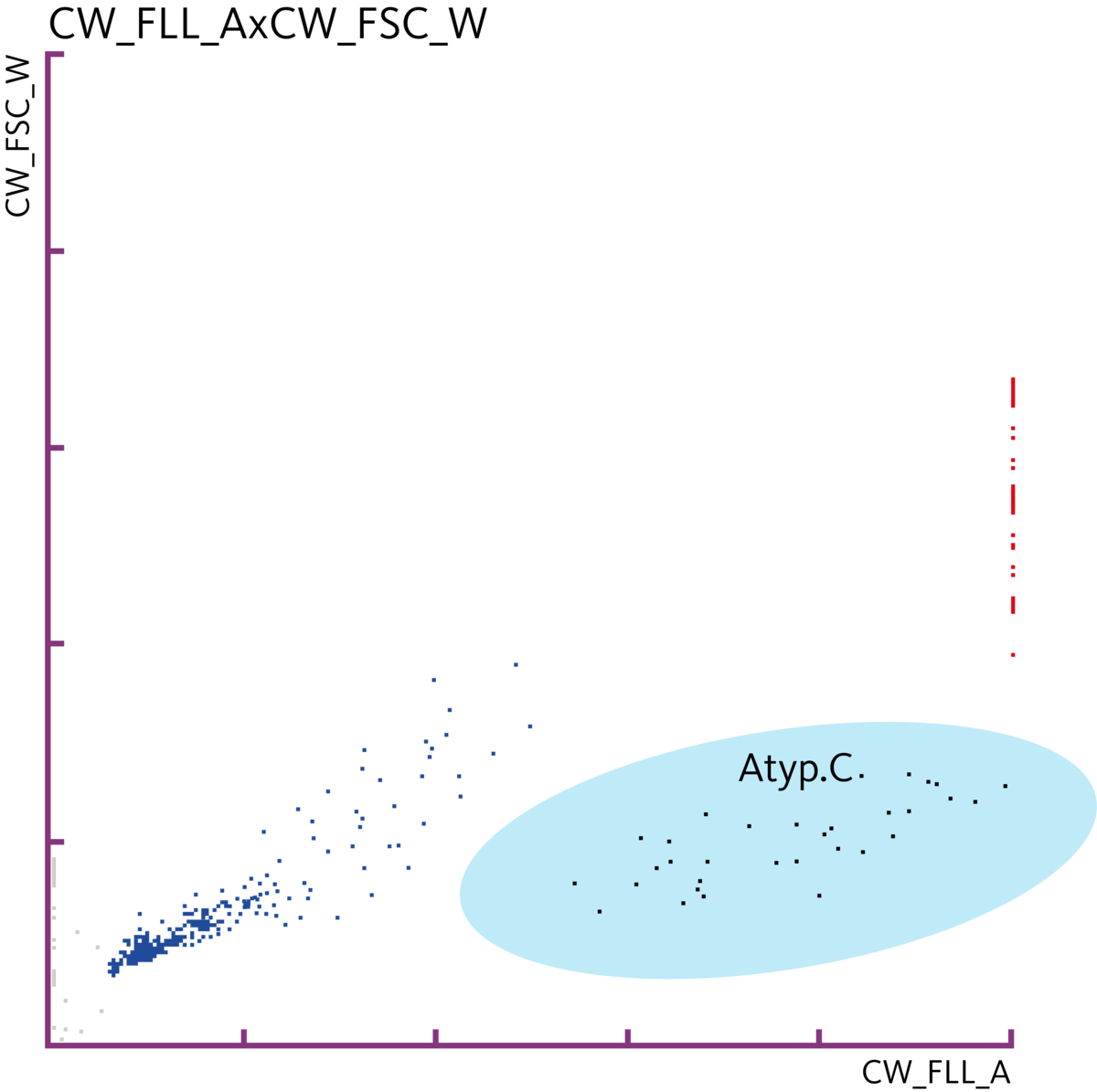
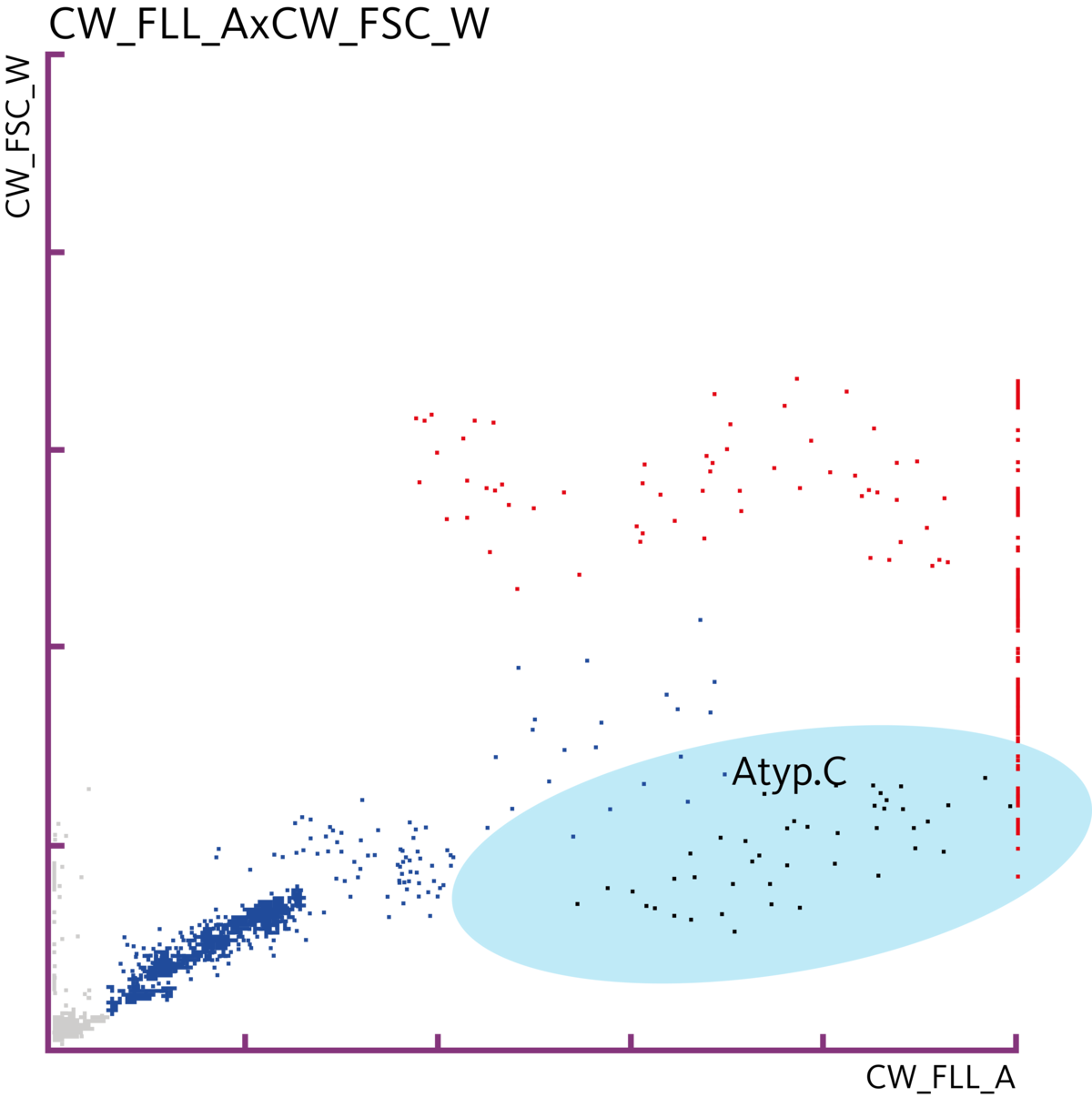
The research parameter Atyp.C allows for the detection of urinary atypical cells as an indicator of a urothelial malignancy. Cellular characteristics such as size, enlarged nuclei and increased nucleocytoplasmic ratios are considered to separate atypical cells from nucleated, non-atypical cells, such as WBC and transitional epithelial cells.
Atyp.C is a research parameter on the UF-Series and allows for the detection of urinary atypical cells and differentiation from non-atypical cells through urinary flow cytometry in correlation with an increased nucleic acid content.
Bladder cancer diagnostics in research
Aydin et al. demonstrated the potential of the UF-series in detection of urothelial malignancies in a case of a recurrent high-grade urothelial carcinoma in an outpatient setting. The use of the UD-10 automated microscope supported these findings.
Tınay et al. revealed the potential to avoid invasive cystoscopies on patient side and to save costs for unnecessary treatments in a heterogenous study population. With an acceptable sensitivity of 75 % and a specificity of 100%, the UF-5000 demonstrated potential value for diagnostic decisions for patients with low-risk non-muscle invasive bladder cancer (NMIBC). For patients with high-risk NMIBC, sensitivity and specificity values are lower, but comparable or even better, if compared to cytology.
Ren et al. demonstrated the predictive power Atyp.C for patients with a suspected diagnosis of urothelial carcinoma. The Atyp.C findings were in agreement with cytopathology in 73 % of the investigated cases. In conclusion, Atyp.C to be used as an accessory test for urothelial carcinomas in context of routine urinary diagnostics, to identify high-risk patients for a more specific follow-up and medical treatment.
Atyp.C in bladder cancer detection
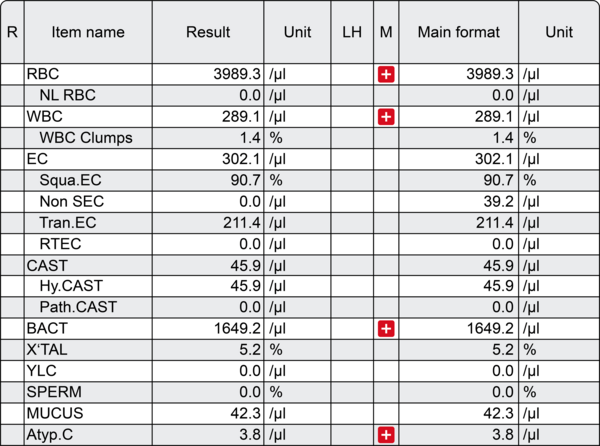
A 71-year-old male patient reports to the clinics with diverse symptoms including fatigue, fever, abdominal pain and macrohaematuria. Several tests were ordered, and among them was the analysis of a fresh urine specimen.
The results from routine urinalysis performed on the UF-5000 confirmed a macrohaematuria with an RBC count of 3,989 cells/µL. The RBC Info ‘Dysmorphic RBC?’ indicates a non-glomerular origin for the haematuria. In addition, the presence of 1,649 bacterial cells/µL indicates a bacterial urinary tract infection, which is accompanied with mild leucocyturia as highlighted by the WBC count of 289 cells/µL. The UF-5000 also detected atypical cells through the Atyp.C research parameter at a concentration of 3.8 cells/µL. All findings were confirmed by the UD-10 automated imaging device.
A cystoscopy was conducted based on these diagnostic findings and insights from the patient anamnesis that highlighted an age of above 70 years, over 40 years of heavy smoking and previous work in the chemical industry. Finally, the cystoscopy revealed the presence of papillary structures that were protruding into the lumen of the bladder, leading to the diagnosis of bladder cancer.
Atyp.C in bladder cancer surveillance
A 75-year-old male patient reports to his general practitioner for a routine check-up. He has a medical history of type-2 diabetes and was treated for non-muscle invasive bladder cancer three years ago. The tumour was removed then by transurethral resection. Continuous bladder cancer surveillance by cystoscopy, last carried out nine months ago, did not reveal any recurrence of the bladder tumour.
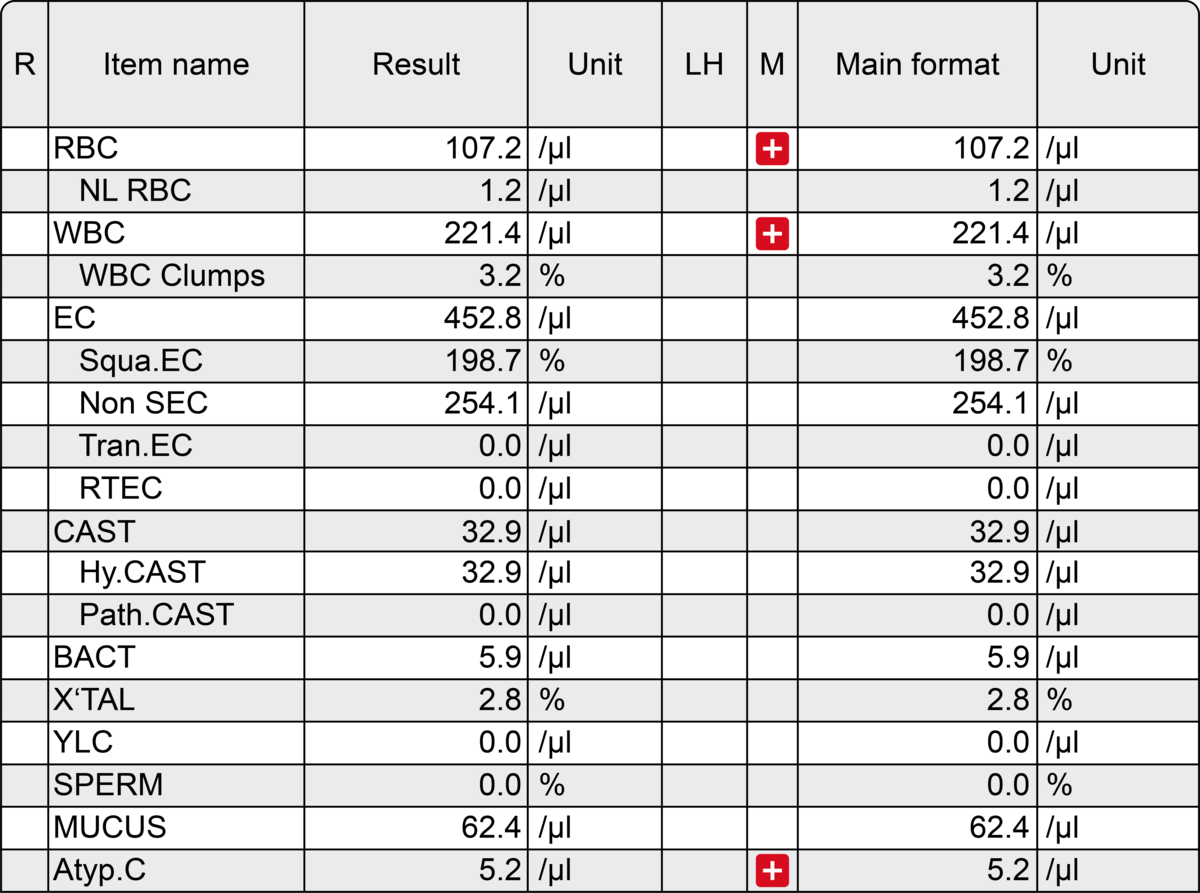
A standard urinalysis through urinary flow cytometry on the UF-5000 revealed slight indications for haematuria of non-glomerular origin and leucocyturia by the presence of 107 RBC/µL and 221 WBC/µL, respectively. There was no indication for a bacterial infection of the urinary tract. However, atypical cells, which was detected by the research parameter Atyp.C, were present at a concentration of 5.2 cells/µL.
Based on the diagnostic findings and the previous presence of urothelial carcinoma, a cystoscopy was conducted, confirming the recurrence of a bladder tumour through the presence of papillary structures.
Scientific references
[1] Aydin, O. (2021): Atypical cells parameter in Sysmex UN automated urine analyzer: feedback from the field. Diagn Pathol
[2] Ren, C., Wang, X., Yang, C. et al. (2020): Investigation of Atyp.C using UF-5000 flow cytometer in patients with a suspected diagnosis of urothelial carcinoma: a single-center study. Diagn Pathol
[3] Sanli, O., Dobruch, J., Knowles, M. et al. (2017): Bladder cancer. Nat Rev Dis Primers
[4] Tınay İ , Şahin B, Saraçoğlu S et al. (2019): “Atypical Cell’’ Parameter in Automated Urine Analysis for the Diagnosis of Bladder Cancer: A Retrospective Pilot Study. Bull Urooncol
![[.ZA-en South Africa (english)] Atypical cells can be detected using clinical flow cytometry technology. Laboratory and clinicians](/fileadmin/_processed_/d/6/csm_Bladder_cancer_clinicians_and_laboratory_4362aca72d.jpg)